Table of Contents
ToggleCeliac disease might sound like a fancy term you’d hear at a gluten-free bakery, but it’s much more serious than that. Imagine your body throwing a tantrum every time you munch on a slice of bread. That’s what happens when someone with celiac disease encounters gluten. But is celiac really an autoimmune disease? Spoiler alert: yes, it is, and it’s not just a fad diet for the health-conscious.
Understanding Celiac Disease
Celiac disease is a chronic autoimmune disorder that affects the digestive system. The condition arises when the immune system mistakenly attacks the small intestine due to gluten, a protein found in wheat, barley, and rye. Symptoms can vary widely, ranging from gastrointestinal issues like bloating and diarrhea to neurological symptoms and skin rashes.
Individuals with celiac disease often face long-term health consequences if they continue to consume gluten. Damage to the intestinal lining prevents proper nutrient absorption, leading to complications such as anemia, osteoporosis, and increased risk of certain cancers. Testing for celiac disease typically involves blood tests to measure specific antibodies and an intestinal biopsy for definitive diagnosis.
Genetics plays a significant role in celiac disease. About 30% of the population carries the genes associated with the condition, yet only 1% will develop it. Family history significantly increases the risk, making it essential for first-degree relatives of affected individuals to undergo testing.
Dietary management remains the cornerstone of treatment. A strict, lifelong gluten-free diet allows the intestine to heal. While initially challenging, many find support through celiac disease organizations and gluten-free communities.
Research continues to evolve, exploring potential treatments beyond dietary restrictions. Interest is growing in therapies that might modify the immune response to gluten. Understanding celiac disease’s nature will improve awareness and promote early diagnosis, significantly enhancing quality of life for those affected.
The Autoimmune Response
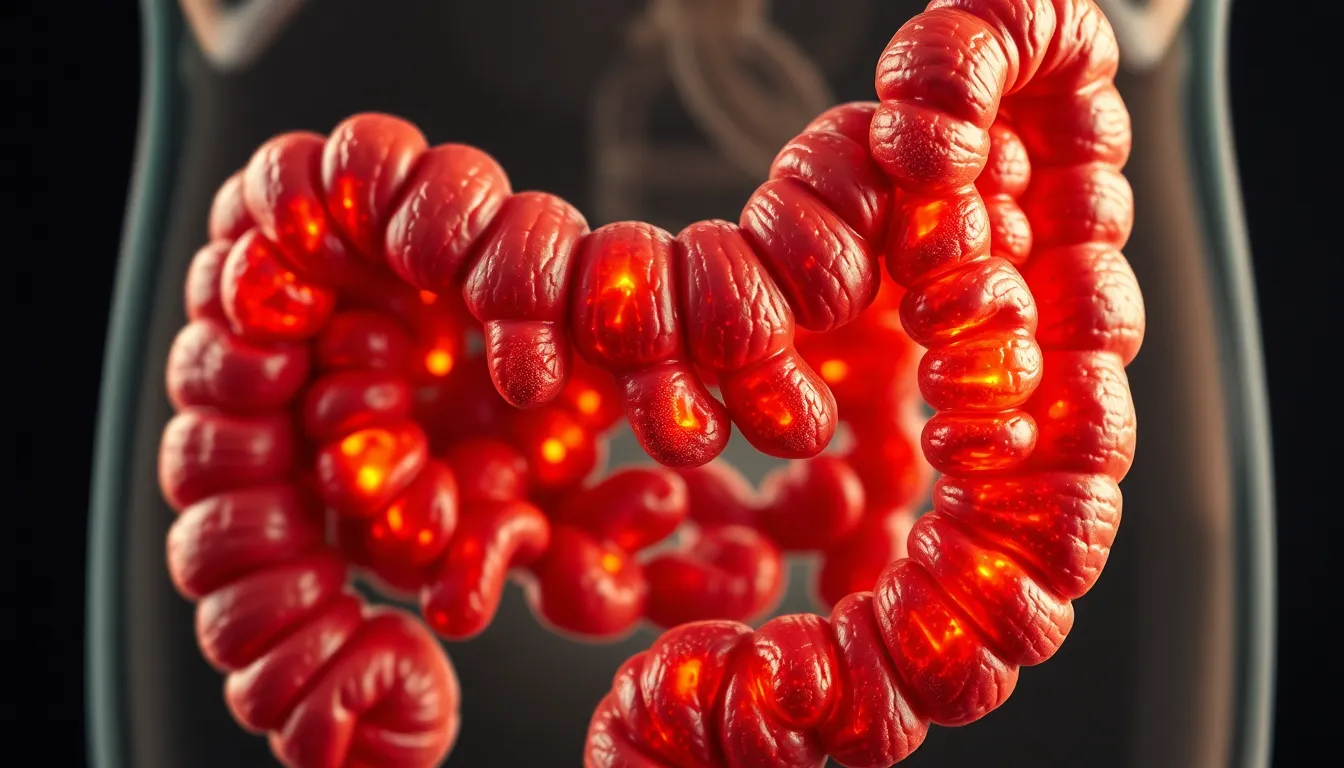
Celiac disease involves a complex autoimmune response triggered by gluten consumption. This response leads to inflammation and damage in the small intestine.
How the Immune System Works
The immune system consistently protects the body from harmful substances. It identifies foreign invaders and launches an attack. In celiac disease, the immune system mistakenly recognizes gluten as a threat. This mistake results in the immune system attacking the small intestine instead of just eliminating gluten. Consequently, inflammation occurs, leading to intestinal damage. The small intestine struggles to absorb essential nutrients due to this ongoing assault.
Triggers of Autoimmunity in Celiac Disease
Multiple factors contribute to the onset of autoimmune responses in celiac disease. Genetic predisposition significantly plays a role, with individuals carrying specific gene variants facing higher risks. Environmental factors also trigger symptoms, particularly the introduction of gluten into the diet. Infections, particularly viral ones, may influence the development of celiac disease in genetically susceptible individuals. Antibiotics can disrupt gut microbiota, potentially exacerbating the risk. Recognizing these triggers is vital for understanding the disease and its management.
Symptoms and Diagnosis
Celiac disease manifests through a variety of symptoms affecting different body systems. While individuals may experience gastrointestinal issues, others might present with neurological symptoms or skin rashes. Recognizing these signs is essential for timely diagnosis and management.
Common Symptoms of Celiac Disease
Symptoms typically include diarrhea, abdominal pain, bloating, and unintended weight loss, which reflect the digestive complications. Many experience fatigue or weakness due to nutrient malabsorption. Skin conditions such as dermatitis herpetiformis can develop, characterized by itchy, blistering rashes. Osteoporosis or anemia arises from long-term nutrient deficiencies. Psychological symptoms, including depression and anxiety, also occur frequently in those with the disease.
Diagnostic Procedures
Diagnosis relies on specific medical tests. Blood tests measure antibodies, such as tissue transglutaminase antibodies, linked to celiac disease. An intestinal biopsy often follows, where small tissue samples from the intestine reveal damage to villi. Genetic tests can identify associated genes in individuals, aiding diagnosis. Regular monitoring and follow-up care ensure management of symptoms and health impacts.
Treatment and Management
Celiac disease management primarily involves adhering to a gluten-free lifestyle. Implementing dietary changes significantly impacts symptom relief and overall health.
Dietary Changes
A strict gluten-free diet remains the cornerstone of treatment. Individuals with celiac disease must eliminate all sources of gluten, which includes avoiding wheat, barley, and rye. Focus on consuming safe alternatives like rice, corn, and quinoa. Incorporating fresh fruits, vegetables, lean proteins, and gluten-free grains ensures balanced nutrition. Label reading is essential; not all processed foods are gluten-free. Cross-contamination poses a risk during food preparation, making dedicated cooking spaces important. Regular consultations with dietitians enhance dietary adherence and nutritional adequacy.
Long-term Health Implications
Long-term adherence to a gluten-free diet can prevent serious health complications associated with celiac disease. Risks of osteoporosis, anemia, and certain cancers decrease with proper management. Maintaining a healthy gut promotes nutritional absorption, leading to improved energy levels and weight stabilization. Regular monitoring of blood levels for deficiencies ensures early intervention. Psychological well-being often improves as individuals can experience reduced anxiety and social isolation. Ongoing research highlights potential therapies that could modify immune responses, but dietary management remains primary for effective disease control.
Celiac disease is a serious autoimmune condition that requires careful management through a strict gluten-free diet. Understanding its complexities is vital for those affected and their loved ones. By recognizing the symptoms and seeking appropriate testing, individuals can take proactive steps toward better health.
The commitment to a gluten-free lifestyle not only alleviates symptoms but also protects against long-term complications. As research continues to advance, raising awareness about celiac disease remains crucial for improving diagnosis and treatment options. Embracing a supportive community can make a significant difference in navigating this challenging condition.







